The Case
Generally, I like to write about positive ultrasound cases. This is not one of those cases. But out of this sad case there was much learning to be had for this med student. At the time of the case, I was on an emergency ultrasound elective. And I couldn’t have be happier! I was learning all sorts of awesome and useful skills. Another perk of being on ultrasound duty was that I got to tag along on all the ultrasound cases I can get my hands on, including the traumas (a big perk in my book). As soon as I heard a trauma called in, I gowned up, gloved up, goggled up, and masked up. I observed the FAST exam (Focused Abdominal Scan for Trauma) and helped however I was instructed. Mostly squeezing IV bags or fetching things, but I was in there; I had a job; and I was learning ultrasound awesomeness. Life was good…. like really, really good. Until it wasn’t. Enter a teenager in an ATV accident. One paramedic cranks out compressions, while the other relays patient information. Car versus ATV. Trouble intubating. And he’s asystolic. Huge bummer. This is not going to be fun and someone somewhere is going to be very sad tonight. Everyone is hustling. I stand at the foot of the bed squeezing fluids into the kid while lines are placed, drugs are pushed, and they figure out what’s wrong. I watch the FAST exam. Looks negative to me, so no visible blood in the pelvis, abdomen, or around the heart. Unfortunately the ultrasound’s heart view also shows no heart movement. There is no electrical activity on the ECG. He’s been down for a long time. Time of death is called. Everyone puts down what they were doing and steps away. I feel heavy. After the room has cleared, the ultrasound attending pulls the ultrasound up to the bedside. There is a valuable teaching opportunity here. He does another FAST exam, explaining it as he goes. Still no free fluid in the pelvis, abdomen, or pericardium. He puts the probe on his chest. No signs of pneumo or hemothorax. This is weird; an ATV versus car with no major bleeding from the neck down. I’m supposed to be learning what an ultrasound exam looks like on a trauma patient, but so far it all looks pretty normal. That’s odd… so what killed this kid? The ultrasound attending agrees it’s unusual and wants to check one more thing. Here’s where things get interesting. The only visible trauma is from the neck up; some bleeding from the ears, eyes, and an open scalp lac. With no helmet that really isn’t a surprise. What is a surprise is the ultrasound attending putting the ultrasound probe on his eye. What are we suppose to tell from this..? Intracranial pressure. Mind blow. Now I’m pretty sure the ultrasound attending is a wizard. On the screen, we see a normal globe with a huge optic nerve and sheath exiting. Before he even measures it, he can tell it’s too big. He measures it and confirms ICP is elevated. So how’d he do this?
Measuring Intracranial Pressure Using Ocular Ultrasound
In a Nutshell
- If you suspect elevated intracranial pressure (ICP), ocular ultrasound is a fast and easy method to detect it.
- You can measure the optic nerve sheath diameter (ONSD) using ultrasound.ONSD > 5 mm may indicate an ICP > 20 mmHg, especially in symptomatic patients.
- Not everyone with ONSD > 5 mm has elevated ICP.
- ONSD > 5.7 mm indicates an ICP > 20 mmHg.
- All patients with ONSD > 5.7 mm have elevated ICP.
The Method Setting up:
- Put a generous amount of ultrasound gel on the eye.
- Put on enough gel, so you don’t put ANY pressure on the eye when the probe is applied to the gel. Think of the probe floating above the eye in the gel.
- Ultrasound gel is safe to put on eyes and won’t hurt the patient if some gets in their eyes.
- Select the linear probe and apply it to the gel.
- Don’t push on the eye!
- Rest your hand on a bony structure (like the patient’s eye brow or bridge of their nose)
- This will stabilize your hand and the image.
What You’ll See:
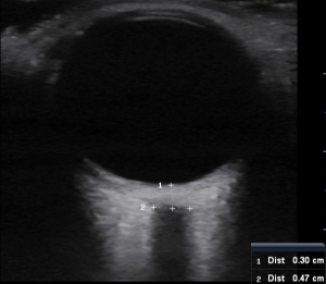
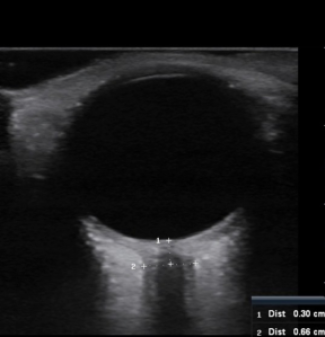
- You’ll see the globe of the eye at the top of the screen and the optic nerve exiting the globe at the bottom of the screen.
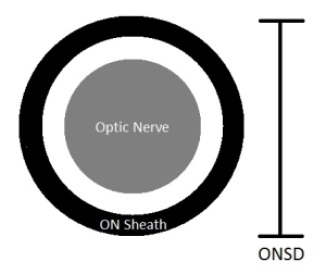
- The optic nerve is a homogenous, hypoechoic (dark grey) area.
- The optic nerve sheath is more reflective, so it’s brighter than the optic nerve.
Measuring ONSD:
- There is a caliper function on ultrasound machines that gives you precise measurements of selected structures.
- Take your ONSD measurement 3 mm posterior to the globe.
- This area has the greatest contrast with surrounding tissue (more contrast = more accurate measurements).
- Use the calipers to determine 3 mm.
- Measure across the optic nerve sheath (not just the optic nerve).
- Measure ONSD for both eyes and average the two measurements.
Interpreting Your Results:
- Increased ONSD correlates with increased ICP
- Upper limit of normal ONSD vary with age…
- Adults: < 5 mm
- Children > 1 yo: < 4.5 mm
- Children < 1 yo: < 4 mm
- ONSD 5 – 5.7 mm: may indicate ICP > 20 mmHg, especially if symptomatic
- > 5 mm is 100% sensitive for elevated ICP
- All patients with elevated ICP have ONSD > 5mm
- ONSD > 5.7 mm: indicates ICP > 20 mmHg
- > 5.7 mm is 100% specific for elevated ICP
- Only patients with elevated ICP have ONSD > 5.7 mm
- ONSD measurements increase with increasing ICP.
- ONSD measurements plateau around 7.5 mm even with significantly increased ICP.
- In severe cases, an echoluscent circle called a crescent sign may be present.
- Crescent sign is formed by the separation of the optic nerve sheath from the optic nerve by high ICP.
Relevant Anatomy: What Makes the Magic Happen?
The optic nerve is surrounded by an optic nerve sheath. The optic nerve sheath connects with the subarachoid space. Because it is also easily distensible, increases in intracranial pressure lead to dilation of the optic nerve sheath. Since the optic nerve and its sheath are easily visualized on ultrasound, an estimate of intracranial pressure can be determined quickly and noninvasively. For trauma patients, this is especially useful. In the trauma patient with a positive FAST exam being hurried to the OR, ICP can be quickly evaluated without delaying treatment. The need for a head CT or early involvement of neurosurgery can then be addressed early and reduce the likelihood of a bad neurological outcome. An important anatomical point to note is that you are scanning over the eye. If your patient is conscious, pressing on the eye may cause pain. If your patient sustained a trauma consistent with head injury and elevated ICP, they might also have ocular trauma (ruptured globe, etc). Be aware of this and be cautious when applying the ultrasound probe to the eye. Pressing on the eye may cause further damage or cause pain in the conscious patient, so apply enough gel that the probe floats above in the eye in a pillow of gel.
Measurements in Doubt? Do the Thirty Degree Test!
- Perform same procedure as above, having the patient gaze thirty degrees from center.
- This will stretch the optic nerve and sheath length-wise, causing fluid to be distributed within the extended sheath.
- If ICP is elevated, ONSD will decrease compared to your original ONSD measurement.
- If ONSD is enlarged for other reasons (like optic nerve thickening or parenchymal infiltration), ONSD diameter will remain similar to your original measurement.
Show Me the Evidence!
What the Emergency Medicine Folks Say…
- Prospective, blinded study of 35 patients comparing ONSD ultrasound to head CT as a predictor of elevated ICP.
- Used ONSD > 5mm for predicting elevated ICP in patients suspected of having elevated ICP (symptomatic).
- When compared with CT, ONSD ultrasound was 100% sensitive and 95% specific for detecting elevated ICP. Awesome!
- ONSD > 5 mm in symptomatic patients is a good predictor of elevated ICP.
What the Critical Care Folks Say…
- Prospective, blinded study of 76 critical care patients (50 with brain injury and 26 controls) correlating ONSD and non-invasive ICP measurements (traditional neuroimaging).
- In brain injury patients ONSD strongly correlated with traditional ICP monitoring values. Fantastic! And it could tell increased ICP patients from healthy controls.
- They did some fancy calculations and determined an ONSD > 5.7 mm was 100% specific and 74% sensitive for predicting elevated ICP. This means…
- All patients with ONSD > 5.7 mm had elevated ICP.
- But using 5.7 mm as your cut-off value would miss 26% of patients with elevated ICP. Obviously no bueno.
What the Neurointensivist Folks Say…
- Prospective, blinded study of 65 neuro ICU patient with 536 ONSD measurements collected over time comparing ONSD ultrasound to more invasive ICP monitoring.
- In severe brain injured patients ONSD correlates with invasive ICP monitoring and responses to changes in ICP in real-time. This is some good stuff here.
What Does It All Mean?
- ONSD > 5 mm: be concerned about elevated ICP, especially in a symptomatic patient.
- If you use this value as your threshold you will catch all elevated ICP patients. That’s good.
- But you’ll also get a couple patients in the mix who don’t have elevated ICP. That’s a little less good.
- ONSD 5 – 5.7 mm is a grey area.
- In this range the patients you suspect have elevated ICP do have it.
- But if you’re practicing on your buddy and their ONSD is > 5 mm, don’t freak out just yet.
- Again, symptoms matter!
- ONSD > 5.7 mm: ICP is elevated.
- You are free to freak out now.
Back to Our Patient
Asystole. ATV versus car. No helmet and physical evidence of head injury (bleeding from eyes and ears). No significant bleeding in the pelvis, abdomen, or chest. Using ultrasound we quickly determined his optic nerve diameter is 5.4 mm. What do you think is going on? Let’s apply the guidelines we just learned…
- Upper limit of normal ONSD is 5 mm.
- ONSD > 5mm in a symptomatic patient is 100% sensitive for ICP > 20 mmHg.
- Patient presents with ONSD of 5.4 mm and is very symptomatic.
- The patient’s ICP is > 20 mmHg!
Based on this information, it appears the patient’s primary injury was probably a head injury. His intracranial pressure was significantly elevated and there was no visible evidence of other injury. This makes the case even sadder. A teenager with no helmet dies of a head injury. That sounds like a preventable death to me. What a waste. The lesson to be learned here is twofold. Always, always wear a helmet! And optic nerve sheath diameters are a quick, reliable, and noninvasive way to measure intracranial pressure.
Other Resources
Both of these Podcasts are a great listen! I highly recommend them if you want to learn more about ultrasound and intracranial pressure. Ultrasound Podcast “Ocular Ultrasound” EMCrit “Increased Intra-Cranial Pressure (ICP) and Herniation, aka Brain Code”
References
Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003;10:376–381.
Blaivas M., Lyon M. (2008). Chapter 17. Ocular Ultrasound.
M. Blaivas, O.J. Ma, J.R. Mateer (Eds), Emergency Ultrasound, 2e. Retrieved October 14, 2012 from http://www.accessemergencymedicine.com/content.aspx?aID=102878.
Fox, Chris; Dawson, Matt. auth. “Ocular Ultrasound with Chris Fox.” Ultrasound Podcast. N.p., 30 2012. web. 14 Oct 2012. http://www.ultrasoundpodcast.com/2012/04/episode-26-ocular-ultrasound-with-chris-fox/>.
Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocritical Care. 2011;15(3):506–515.
Soldatos T, Chatzimichail K, Papathanasiou M. Optic nerve sonography in the diagnostic evaluation of adult brain. Crit Care. 2008;12:R67. doi: 10.1186/cc6897.
Soldatos T, Chatzimichail K, Papathanasiou M, Gouliamos, A. Optic nerve sonography: a new window for the non-invasive evaluation of intracranial pressure in brain injury. Emerg Med J 2009;26:9 630-634.
Weingart, Scott, auth. “Increased Intra-Cranial Pressure (ICP) and Herniation, aka Brain Code.” EMCrit. N.p., 22 2012. web. 14 Oct 2012. http://emcrit.org/podcasts/high-icp-herniation/>.

Jenna, if this is your handiwork on ICP and ocular ultrasound…it is beyond helpful!! thanks!
*Jennifer
Michael, this is my handiwork. I’m SO glad you found it helpful!! Thank you for your kind comment! Happy ultrasounding!
Jennifer